Diabetic Foot Ulcer – Clinical Trial Feasibility

Foot ulcers refer to a patch of broken-down skin usually on the lower leg or feet. In diabetics, when blood sugar levels are high or fluctuate regularly, skin that would normally heal may not properly repair itself because of nerve damage. therefore start a foot ulcer.
It occurs in 15% of people with diabetes and precedes 84% of all diabetes-related lower-leg amputations.
What is a diabetic foot ulcer?
A diabetic foot is a foot that exhibits any pathology that results directly from diabetes mellitus or any long-term complications of diabetes mellitus.
A diabetic foot ulcer is a major complication of diabetes mellitus and probably the major component of the diabetic foot.
Prevalence of diabetic foot ulcer
- Globally, diabetic foot ulcer prevalence is 6.3% in total diabetic patients, which was higher in males (4.5%) than in females (3.5%), according to a study.
- It was also found that occurrence was higher in type 2 diabetic patients (6.4%) than in type 1 diabetics (5.5%).
- North America had the highest prevalence (13.0%), Oceania had the lowest (3.0%), and the prevalence in Asia (5.5%), Europe (5.1%), and Africa (7.2%).
- Belgium has the highest prevalence (16.6%), followed by Canada (14.8%), the USA (13.0%) and Australia have the lowest (1.5%). [3]
High prevalence of Diabetic Foot Ulcer in North America is well supported by highly motivated and experienced investigators and sites willing to undertake clinical trials in this segment.
A recent clinical trial feasibility on Credevo conducted in the United States received more than 1000% of required responses, before the feasibility had to be closed.
See more details below.
Pathology
- A key feature of wound healing is the stepwise repair of lost extracellular matrix (ECM) that forms the largest component of the dermal skin layer, but in some cases, certain disorders or physiological insult disturbs the wound healing process.
- Diabetes mellitus is one such metabolic disorder that impedes the normal steps of the wound healing process.
- Many studies show a prolonged inflammatory phase in diabetic wounds, which causes a delay in the formation of mature granulation tissue and a parallel reduction in wound tensile strength
Types of Diabetic foot ulcers
Diabetic foot ulcers are classified as either
- Neuropathic
- Neuroischaemic
- Ischaemic
Risk factors
- Poor glycemic control
- Infection
- Older age
- Diabetic neuropathy and/or peripheral vascular disease
- Cigarette smoking
- Previous foot ulcerations or amputations
- Ischemia of small and large blood vessels
- Renal failure and/or edema
Diagnosis
Considerations in the diagnosis of diabetic foot ulcers include the location of the ulcer, Size, shape. and Depth and whether the tissue is granulating or sloughy needs to be considered.
Further considerations include
- Whether there is malodor.
- Investigating the condition of the border of the wound, palpable bone, and sinus formation.
- Signs of infection, such as the development of grey or yellow tissue, purulent discharge, unpleasant smell, sinus, undermined edges, and exposure of bone or tendon.
Treatment plans
Based on the condition and severity, the treatment approach varies and follow as below
Tissue Debridement
Wound debridement or the removal of necrotic tissue from a wound, will reduce pressure, stimulate wound healing, allow for the inspection of underlying tissue, help with secretion or wound drainage and optimize wound dressings’ effectiveness.
Infection Control
- Both oral and topical antibiotics are recommended for all diabetic wound treatment.
- Topical antimicrobials can reduce bacteria, protect against further contamination, and prevent the spread of infection deeper into the wound.
- Typical wound dressings used in treating diabetic wounds are those impregnated with antimicrobial agents to help fight infection.
Moisture Balance
- Choosing the optimal dressing for a diabetic wound is essential to successful wound healing.
- The proper wound dressing will help maintain a balanced moisture environment (not too wet or too dry) and allow the wound to drain and heal properly.
- Some common dressings that can be used for diabetic wounds include Alginates, Hydrocolloids, and Films.
Underlying Factors
A diabetes wound patient must be treated holistically in order to identify underlying issues and reduce risk factors that are causing wounds in the first place.
- Achieving control of diabetes proper nutrition,
- Controlling high blood pressure, and
- Smoking cessation.
Other factors, such as proper footwear and adequate blood supply to extremities, need to be assessed. [2]
Clinical Trials on Diabetic foot ulcer worldwide
A total of 629 Clinical trials on Diabetic foot ulcers are registered around the world, where major studies are from United States (258), United Kingdom (43), France(42), and Canada (30).
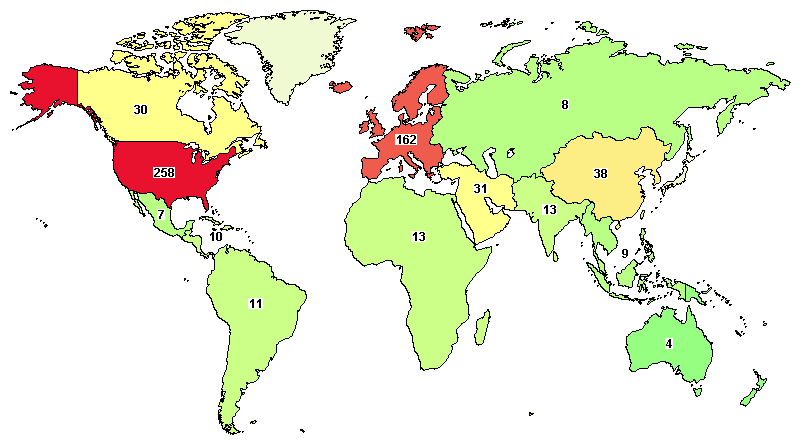
Total on-going trials around the world are 106, in which major studies are in the United States (51), United Kingdom (7), France (9), and Canada (5).
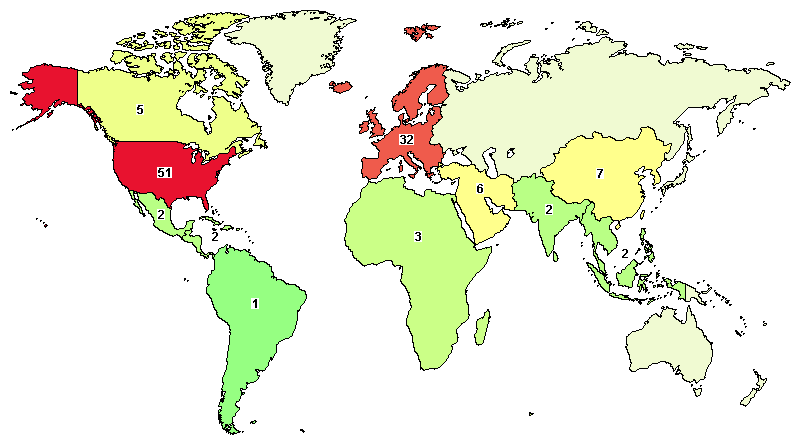
(Data as of 28-Oct-2020)
Feasibility for a randomized, comparator-controlled, double-blind, multicenter phase-II trial in patients with Diabetic Foot Ulcers was conducted recently on Credevo.
Would you like to contact these investigators and assess feasibility with them for your clinical trial?
Check details below.
Feasibility of diabetic foot ulcer in CREDEVO
A randomized, comparator-controlled, double-blind, multicenter phase-II trial was conducted in credevo in order to evaluate the efficacy and safety of the study drug in subjects with Diabetic Foot Ulcer.
The clinical study was conducted in medical centers and sites located in the United States.
The patient population included male or female subjects between 18 and 80 years of age, diagnosed with Type I or Type II diabetics and has diabetic foot ulcers (with no signs of clinical infection) for longer than 4 weeks at the screening visit.
Feasibility results
The trial feasibility received overwhelming responses from medical centers and sites in the United States. Total responses received were more than 1000% of the number of sites actually sought for this trial.
Feasibility data showed that not only there are many experienced and willing sites in the United States for such clinical trials, but, more importantly, these sites actually had a lot of patients possible to be recruited there. The recruitment rate projection obtained from this trial was beyond expectations.
Due to an overwhelming response, the feasibility was closed ahead of time.
Here are the salient results obtained from this feasibility
- Total responses received: >1000% of site requirement
- Average recruitment rate projection: 7 patients/site/month
- Highest recruitment rate reported: 50 patients / month
Contact Investigators From This Feasibility Assessment
Would you like to contact these investigators and assess feasibility with them for your clinical trial?
Now, it’s very easy to do so.
Just provide your email below and further details will be sent to you. Don’t worry, your email will not be published or shared.